- Report: #1496155
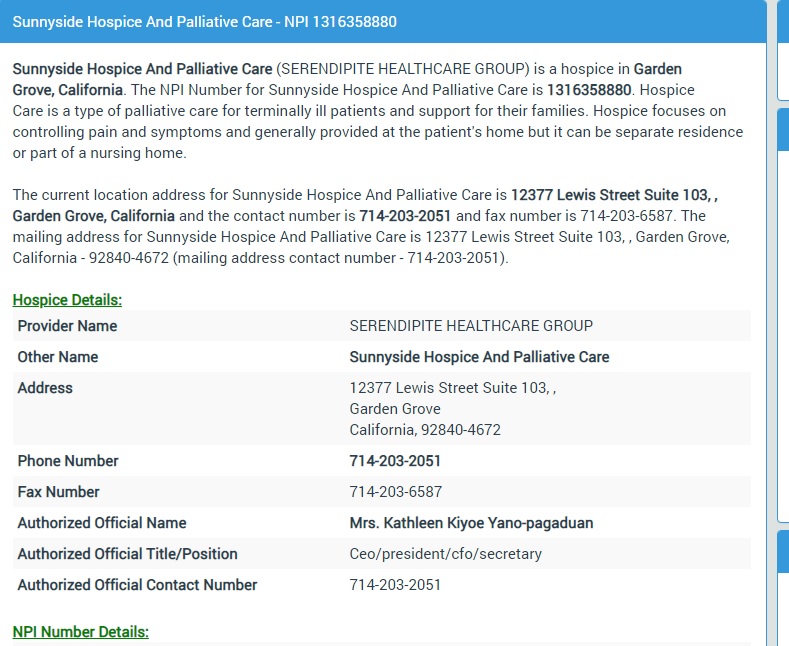
Complaint Review: Sunny Side Hospice in Garden Grove - Gardena Grove Ca
Sunny Side Hospice in Garden Grove Aerol and Kathy SUNNY SIDE HOSPICE BREAKS HIPPA LAWS! Gardena Grove Ca
*Consumer Comment: A bit misdirected
*Consumer Suggestion: Hospice Information
*Consumer Comment: HIPPA and "Covered Entities" Ex: continuation of care AFTER hospitalization
*Consumer Comment: The rebuttals are correct
*Author of original report: Your An Idiot!!! Stacey
*Consumer Comment: Malpractice Info
*Consumer Comment: We are the educated ones...
*Consumer Comment: Angry Girl...You are a rude person!!!
*Author of original report: I don't care
Report Attachments
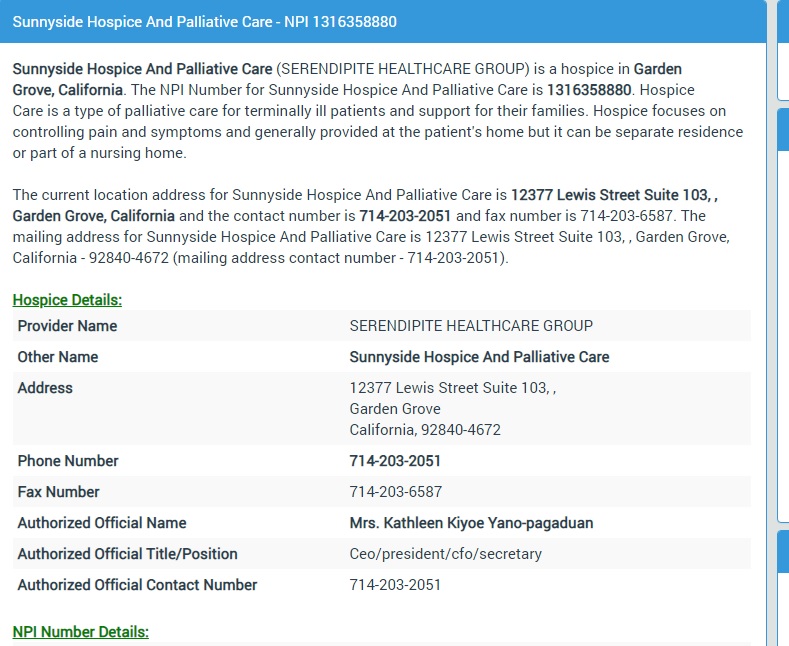

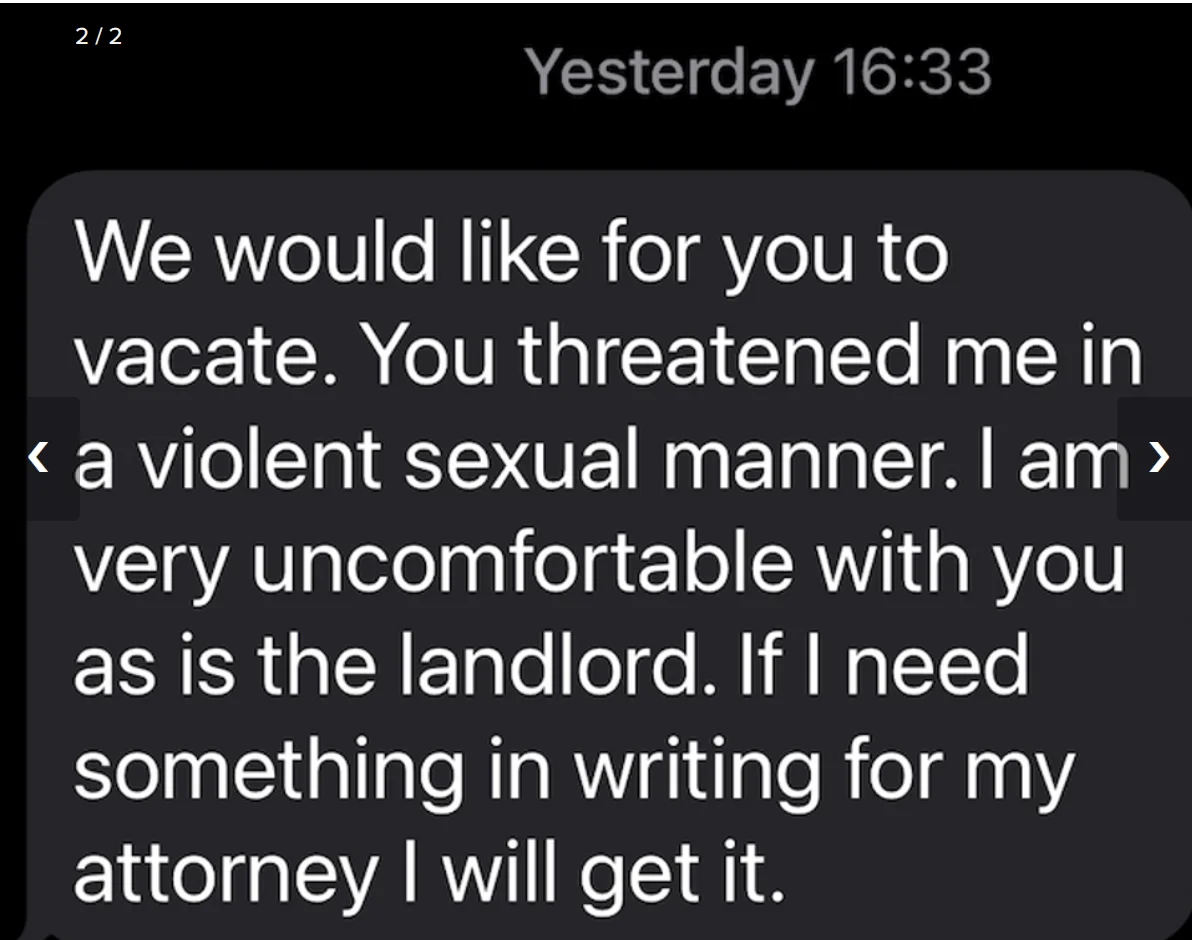
Do NOT trust this company. I briefly spoke to a STUPID girl named Aerol who works for this company. HIPPA LAWS doesn't seem to matter much to this idiot person. As she took it upon herself to ignorantly access my partner's medical records FROM Whittier Hospital without written or verbal authorization from me his POA! I never inquired about this reckless organization's service. A woman named Milcah Escala from Lakeside Hospice gave that dumb Aerol our information. She then calls me, speaks to me for 5 mins and then contacts Whittier without my permission, calls me back, and says he is NOT eligible. Wow both Whittier and Sunny Side are negligent and break HIPPA LAWS Hell, I was never told what the criteria was if any. A person with Dementia not Qualified?? I don't need your sh*t service, no problem, what I do need is a good lawyer to sue this crap company who is owned by this person.

Phone Number 714-203-2051 Fax Number 714-203-6587 Authorized Official Name Mrs. Kathleen Kiyoe Yano-pagaduan Authorized Official Title/Position Ceo/president/cfo/secretary Authorized Official Contact Number 714-203-2051
Aerol didn't care at all what she did, she knew exactly what she was doing. Her ignorant response was "oh I am sorry"... What I do need is a good medical malpractice lawyer to SUE THIS SH*T OUT OF WHITTIER AND SUNNYSIDE HOSPICE.
Do NOT trust this organization!!
9 Updates & Rebuttals
AngryGirl
Hollywood,California,
United States
I don't care
#2Author of original report
Sat, November 14, 2020
Aerol is STUPID AND MORON....you can read my full complaint on AngryGirl Feminist
Aerol broke HIPPA laws its illegal to accessmedical records without permission!!!!!!
Opana
Lappeenranta,Finland
Angry Girl...You are a rude person!!!
#3Consumer Comment
Thu, June 11, 2020
You do not have any valid complaints regarding this Hospice or it's staff. You may be angry, but your hurt feelings and general b*tchyness are not the fault of others. You filed a complaint that called others: "STUPID girl named Aerol", "herself to ignorantly access", " this reckless organization's service" , "gave that dumb Aerol our information", " don't need your sh*t service, no problem, what I do need is a good lawyer to sue this crap company who is owned by this person" Then you call someone who is try explain how this all works as "Ignorant". Is this how you approach all your problems in life? Lash out, blame others, call them names and refuse to learn or educate yourself? Does calling others derogatory names make you feel superior? I sincerely hope that this hospice and its staff see what you have written in RoR. Her's a new word for you: LIBEL What are the 5 basic elements of libel? Under United States law, libel generally requires five key elements: the plaintiff must prove that the information was published, the plaintiff was directly or indirectly identified, the remarks were defamatory towards the plaintiff's reputation, the published information is false, and that the defendant is at fault.
Robert
Irvine,United States
We are the educated ones...
#4Consumer Comment
Thu, June 11, 2020
Hopefully you will be able to take a step back and actually read what people are posting. As NOTHING you posted here shows any HIPAA violations.
Even if they did call you, this wasn't some sort of "Cold Call" with a company just randomly calling people seeing if they may need Hospice Services. There was obviosuly an inquiry for their services from someone, and contrary to what you are thinking it was probably you. Perhaps an e-mail, perhaps entering in a form on a website, perhaps talking to someone at the Hospital if you requested or discussed Hospice. The reasons it is likely not a violation has already been covered and nothing you posted goes against that.
I'm not here to defend them, but more to try and educate you. As while we do feel for your situation, whatever the exact situation is. Going after this(or any Hospice based on your comments) for what is basically non-existant violations is probably not where you should be directing your efforts right now.
Good Luck
Opana
New York,New York,
United States
Malpractice Info
#5Consumer Comment
Thu, June 11, 2020
Good luck on suing the Hospice. Here is additional information on malpractice: To prove that medical malpractice occurred, you must be able to show all of these things: 1. A doctor-patient relationship existed. ... 2. The doctor was negligent. ... 3. The doctor's negligence caused the injury. ... 4. The injury led to specific damages. ... 5. Failure to diagnose. ... 6. Improper treatment. ... 7. Failure to warn a patient of known risks. What are the 4 D's of malpractice? The four Ds of medical malpractice are duty, dereliction (negligence or deviation from the standard of care), damages, and direct cause. Each of these four elements must be proved to have been present, based on a preponderance of the evidence, for malpractice to be found.
Your a Moron!
Hollywood,California,
United States
Your An Idiot!!! Stacey
#6Author of original report
Thu, June 11, 2020
Why don't you educate yourself you fuc*(king moron!
I never requested anything from this shady business NEVER!
Aerol called me I never called her!
Maybe your stupid employee should tell people exactly what she intended to do before actually doing it!
All Hospice are shady and crooked business's!!!!!!
Stacey
United StatesThe rebuttals are correct
#7Consumer Comment
Thu, June 11, 2020
I work with many hospice companies in my role and if your loved one did not have an admitting diagnosis that hospice could substantiate then they are not eligible for hospice service per Medicare/Medicaid guidelines. As for this company violating HIPAA that is not the problem. All hospice companies must comply with all HIPAA regulations in order to be compliant with State and Federal law.
Once a family member/loved one ask for hospice services then that person has allowed the company/hospital/rehab to request an order for hospice consult so that the company can assess the patient for diagnosis and if there need for hospice services. All hospitals have the right to ask for a loved one to fill out the appropriate HIPAA paperwork to share medical information with any indentity that asks for this information. So if you are angry that your loved one was not accepted to hospice then sorry. Subjecting a company to a ROR to destroy their reputation is just a pathetic excuse on your part.
Opana
New York,United States
HIPPA and "Covered Entities" Ex: continuation of care AFTER hospitalization
#8Consumer Comment
Wed, June 10, 2020
You will be unable to win a law suit for breach of privacy from what you stated. Any type of continuity of care (SNF, home care, hospice) after hospitalization always results in information being shared to plan for the next level of care needed by the patient. Check below under "COVERED ENTITIES" and you will see that HIPPA does NOT bar information sharing when appropriate. In this case, it was to communicate & refer to hospice.
Please educate yourself before you get angry. https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/HIPAA-ACA/PrivacyandSecurityInformation Permitted Uses and Disclosures. A covered entity is permitted, but not required, to use and disclose protected health information, without an individual’s authorization, for the following purposes or situations:
(1) To the Individual (unless required for access or accounting of disclosures);
(2) Treatment, Payment, and Health Care Operations;
(3) Opportunity to Agree or Object;
(4) Incident to an otherwise permitted use and disclosure;
(5) Public Interest and Benefit Activities; and
(6) Limited Data Set for the purposes of research, public health or health care operations.18 Covered entities may rely on professional ethics and best judgments in deciding which of these permissive uses and disclosures to make. The Standards for Privacy of Individually Identifiable Health Information ("Privacy Rule”) establishes, for the first time, a set of national standards for the protection of certain health information. The U.S. Department of Health and Human Services ("HHS”) issued the Privacy Rule to implement the requirement of the Health Insurance Portability and Accountability Act of 1996 ("HIPAA”).1 The Privacy Rule standards address the use and disclosure of individuals’ health information—called "protected health information” by organizations subject to the Privacy Rule — called "covered entities,” as well as standards for individuals' privacy rights to understand and control how their health information is used. Within HHS, the Office for Civil Rights ("OCR”) has responsibility for implementing and enforcing the Privacy Rule with respect to voluntary compliance activities and civil money penalties. What are Treatment, Payment, and Health Care Operations?
The core health care activities of "Treatment,” "Payment,” and "Health Care Operations” are defined in the Privacy Rule at 45 CFR 164.501. "Treatment” generally means the provision, coordination, or management of health care and related services among health care providers or by a health care provider with a third party, consultation between health care providers regarding a patient, or the referral of a patient from one health care provider to another. "Payment” encompasses the various activities of health care providers to obtain payment or be reimbursed for their services and of a health plan to obtain premiums, to fulfill their coverage responsibilities and provide benefits under the plan, and to obtain or provide reimbursement for the provision of health care. In addition to the general definition, the Privacy Rule provides examples of common payment activities which include, but are not limited to:
Determining eligibility or coverage under a plan and adjudicating claims; • Risk adjustments; • Billing and collection activities; • Reviewing health care services for medical necessity, coverage, justification of charges, and the like; • Utilization review activities; and • Disclosures to consumer reporting agencies (limited to specified identifying information about the individual, his or her payment history, and identifying information about the covered entity). • "Health care operations” are certain administrative, financial, legal, and quality improvement activities of a covered entity that are necessary to run its business and to support the core functions of treatment and payment. These activities, which are limited to the activities listed in the definition of "health care operations” at 45 CFR 164.501, include: • Conducting quality assessment and improvement activities, population-based activities relating to improving health or reducing health care costs, and case management and care coordination; • Reviewing the competence or qualifications of health care professionals, evaluating provider and health plan performance, training health care and non-health care professionals, accreditation, certification, licensing, or credentialing activities;
Opana
New York,New York,
United States
Hospice Information
#9Consumer Suggestion
Wed, June 10, 2020
I am sorry that your partner was denied Hospice services. The burden of care falls to you, and I can see you are very angry with this facility. Each Hospice must follow the rules as set by CMS. I have cited that information below. Perhaps this will assist you in your quest for Hospice care. Hospice According to Title 18, Section 1861 (dd) of the Social Security Act, the term "hospice care” means the following items and services provided to a terminally ill individual by, or by others under arrangements made by, a hospice program under a written plan (for providing such care to such individual) established and periodically reviewed by the individual's attending physician and by the medical director (and by the interdisciplinary group described in paragraph (2)(B)) of the program—
(A) nursing care provided by or under the supervision of a registered professional nurse, (B) physical or occupational therapy, or speech-language pathology services, (C) medical social services under the direction of a physician, (D)(i) services of a home health aide who has successfully completed a training program approved by the Secretary and (ii) homemaker services, (E) medical supplies (including drugs and biologicals) and the use of medical appliances, while under such a plan,
(F) physicians' services, (G) short-term inpatient care (including both respite care and procedures necessary for pain control and acute and chronic symptom management) in an inpatient facility meeting such conditions as the Secretary determines to be appropriate to provide such care, but such respite care may be provided only on an intermittent, non-routine, and occasional basis and may not be provided consecutively over longer than five days,
(H) counseling (including dietary counseling) with respect to care of the terminally ill individual and adjustment to his death, and (I) any other item or service which is specified in the plan and for which payment may otherwise be made under this title. The care and services described in sub-paragraphs (A) and (D) may be provided on a 24-hour, continuous basis only during periods of crisis (meeting criteria established by the Secretary) and only as necessary to maintain the terminally ill individual at home. §418.22 Certification of terminal illness.
(a) Timing of certification—(1) General rule. The hospice must obtain written certification of terminal illness for each of the periods listed in §418.21, even if a single election continues in effect for an unlimited number of periods, as provided in §418.24(c). (2) Basic requirement. Except as provided in paragraph (a)(3) of this section, the hospice must obtain the written certification before it submits a claim for payment. (3) Exceptions. (i) If the hospice cannot obtain the written certification within 2 calendar days, after a period begins, it must obtain an oral certification within 2 calendar days and the written certification before it submits a claim for payment.
(ii) Certifications may be completed no more than 15 calendar days prior to the effective date of election. (iii) Recertifications may be completed no more than 15 calendar days prior to the start of the subsequent benefit period. (4) Face-to-face encounter. (i) As of January 1, 2011, a hospice physician or hospice nurse practitioner must have a face-to-face encounter with each hospice patient whose total stay across all hospices is anticipated to reach the 3rd benefit period. The face-to-face encounter must occur prior to, but no more than 30 calendar days prior to, the 3rd benefit period recertification, and every benefit period recertification thereafter, to gather clinical findings to determine continued eligibility for hospice care.
(ii) During a Public Health Emergency, as defined in §400.200 of this chapter, if the face-to-face encounter conducted by a hospice physician or hospice nurse practitioner is for the sole purpose of hospice recertification, such encounter may occur via a telecommunications technology and is considered an administrative expense. Telecommunications technology means the use of interactive multimedia communications equipment that includes, at a minimum, the use of audio and video equipment permitting two-way, real-time interactive communication between the patient and the distant site hospice physician or hospice nurse practitioner.
(b) Content of certification. Certification will be based on the physician's or medical director's clinical judgment regarding the normal course of the individual's illness. The certification must conform to the following requirements: (1) The certification must specify that the individual's prognosis is for a life expectancy of 6 months or less if the terminal illness runs its normal course. (2) Clinical information and other documentation that support the medical prognosis must accompany the certification and must be filed in the medical record with the written certification as set forth in paragraph (d)(2) of this section. Initially, the clinical information may be provided verbally, and must be documented in the medical record and included as part of the hospice's eligibility assessment.
(3) The physician must include a brief narrative explanation of the clinical findings that supports a life expectancy of 6 months or less as part of the certification and recertification forms, or as an addendum to the certification and recertification forms. (i) If the narrative is part of the certification or recertification form, then the narrative must be located immediately prior to the physician's signature. (ii) If the narrative exists as an addendum to the certification or recertification form, in addition to the physician's signature on the certification or recertification form, the physician must also sign immediately following the narrative in the addendum.
(iii) The narrative shall include a statement directly above the physician signature attesting that by signing, the physician confirms that he/she composed the narrative based on his/her review of the patient's medical record or, if applicable, his/her examination of the patient. (iv) The narrative must reflect the patient's individual clinical circumstances and cannot contain check boxes or standard language used for all patients. (v) The narrative associated with the 3rd benefit period recertification and every subsequent recertification must include an explanation of why the clinical findings of the face-to-face encounter support a life expectancy of 6 months or less.
(4) The physician or nurse practitioner who performs the face-to-face encounter with the patient described in paragraph (a)(4) of this section must attest in writing that he or she had a face-to-face encounter with the patient, including the date of that visit. The attestation of the nurse practitioner or a non-certifying hospice physician shall state that the clinical findings of that visit were provided to the certifying physician for use in determining continued eligibility for hospice care. (5) All certifications and recertifications must be signed and dated by the physician(s), and must include the benefit period dates to which the certification or recertification applies. (c) Sources of certification.
(1) For the initial 90-day period, the hospice must obtain written certification statements (and oral certification statements if required under paragraph (a)(3) of this section) from— (i) The medical director of the hospice or the physician member of the hospice interdisciplinary group; and (ii) The individual's attending physician, if the individual has an attending physician. The attending physician must meet the definition of physician specified in §410.20 of this sub-chapter. (2) For subsequent periods, the only requirement is certification by one of the physicians listed in paragraph (c)(1)(i) of this section. (d) Maintenance of records. Hospice staff must—
(1) Make an appropriate entry in the patient's medical record as soon as they receive an oral certification; and (2) File written certifications in the medical record. [55 FR 50834, Dec. 11, 1990, as amended at 57 FR 36017, Aug. 12, 1992; 70 FR 45144, Aug. 4, 2005; 70 FR 70547, Nov. 22, 2005; 74 FR 39413, Aug. 6, 2009; 75 FR 70463, Nov. 17, 2010; 76 FR 47331, Aug. 4, 2011; 85 FR 19289, Apr. 6, 2020] §418.25 Admission to hospice care. (a) The hospice admits a patient only on the recommendation of the medical director in consultation with, or with input from, the patient's attending physician (if any).
(b) In reaching a decision to certify that the patient is terminally ill, the hospice medical director must consider at least the following information: (1) Diagnosis of the terminal condition of the patient. (2) Other health conditions, whether related or unrelated to the terminal condition. (3) Current clinically relevant information supporting all diagnoses. [70 FR 70547, Nov. 22, 2005] https://ecfr.io/Title-42/pt42.3.418#se42.3.418_122
Robert
Irvine,United States
A bit misdirected
#10Consumer Comment
Wed, June 10, 2020
It seems as if your real issue with this company is them denying you services for your partner, and that is something between you and them.
But with that, there is really no HIPAA violations for this company asking for information. If there was any violaton, and you haven't really shown that either, it would have been the Hospital because they are the ones who actually provided the information.
It really all depends on the exact circumstances. Such as what paperwork was signed when you admitted your partner to the Hospital. Very often you would also have signed an authorization to share the medical information between different entitites for permissible purposes. Determining eligibility could be seen as permissable. As the hospital didn't just stop someone in the street to tell them your information, they were talking to another entity who you had contacted in order to provide medical services.